
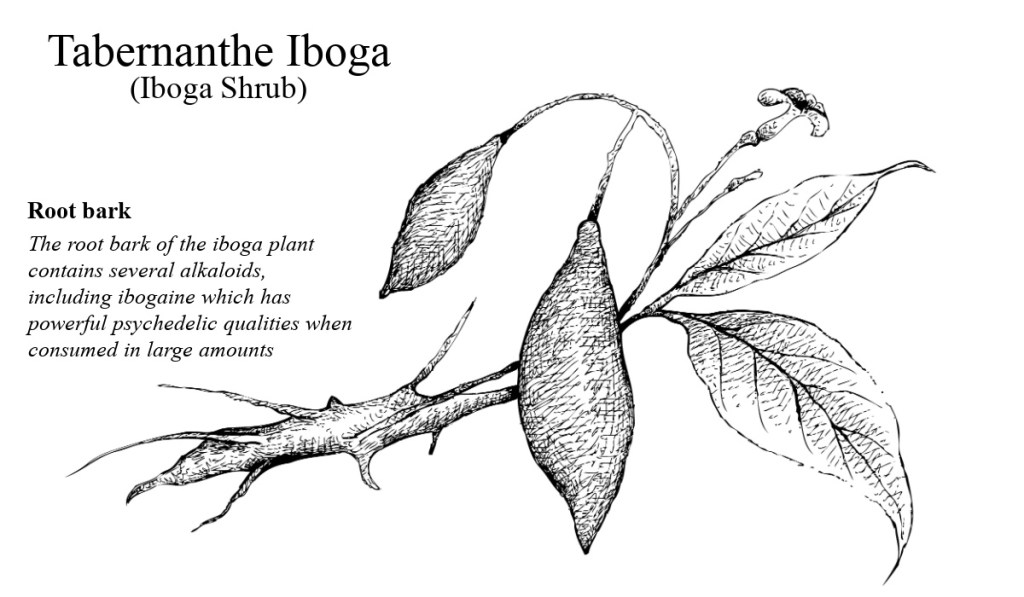
Ibogaine, a naturally occurring psychoactive compound derived from the root bark of the Tabernanthe iboga shrub, has garnered significant attention in recent decades for its potential to treat addiction and substance use disorders. Indigenous to Central and West Africa, ibogaine has a rich history rooted in traditional practices and is now at the forefront of psychedelic therapy research. In Canada, where its legal status remains complex, ibogaine therapy is emerging as a promising yet controversial tool for addressing the opioid crisis and other forms of substance abuse. This article explores the history and benefits of ibogaine, its therapeutic applications, efforts to legalize it in Canada, its sourcing and usage, and its profound effects on addiction recovery.
The History of Ibogaine: From Ritual to Remedy
Ibogaine’s story begins in the rainforests of Central Africa, particularly in Gabon, Cameroon, and the Republic of Congo, where the Tabernanthe iboga plant has been used for centuries by the Bwiti people in spiritual and healing rituals. The Bwiti religion incorporates iboga root bark—chewed or brewed into a tea—as a sacrament in coming-of-age ceremonies and rites of passage, believed to connect practitioners with ancestors and offer profound insights into existence. In small doses, iboga acts as a stimulant, historically used by hunters to enhance alertness and stamina while suppressing hunger and fatigue.
The compound’s introduction to the Western world came in the 19th century when French and Belgian explorers documented its use. By the early 20th century, ibogaine was isolated and marketed in France under the name Lambarène as a stimulant and antidepressant in 8 mg tablets, available until the 1970s. Its psychoactive properties, however, remained largely unexplored in modern medicine until the mid-20th century.

The pivotal moment for ibogaine’s modern reputation came in 1962 when Howard Lotsof, a 19-year-old heroin addict from New York, accidentally discovered its anti-addictive potential. After taking ibogaine recreationally, Lotsof found his cravings and withdrawal symptoms vanished, remaining absent for months. This experience inspired him to advocate for ibogaine as an addiction treatment, filing patents in the 1980s and sparking scientific interest. His work laid the foundation for ibogaine’s transition from a ritualistic substance to a potential therapeutic agent.
Benefits of Ibogaine: A Unique Psychedelic with Anti-Addictive Properties
Ibogaine stands apart from classic psychedelics like LSD, psilocybin, or mescaline due to its dual action: it produces intense psychoactive effects while exerting a pharmacological influence on addiction-related neural pathways. Its primary benefits include:
- Reduction of Withdrawal Symptoms: Ibogaine is renowned for its ability to alleviate the acute physical symptoms of opioid withdrawal, such as nausea, muscle aches, and cravings, often within hours of administration. Unlike traditional detox methods, it offers an “interruption” of withdrawal, providing a window for recovery.
- Craving Suppression: Studies and anecdotal reports suggest ibogaine can diminish substance cravings for weeks, months, or even years after a single dose, a feature attributed to its metabolite, noribogaine, which persists in the body and modulates neurotransmitter activity.
- Neuroplasticity and Psychological Insight: Ibogaine enhances neural plasticity, allowing the brain to “rewire” addiction-related circuits. Users often report a dream-like state during treatment, experiencing vivid autobiographical memories or visions that provide insight into the root causes of their addiction, such as trauma or emotional distress.
- Broad Spectrum Efficacy: Beyond opioids, ibogaine shows promise in treating dependence on alcohol, cocaine, methamphetamine, and nicotine, making it a versatile candidate for addressing polysubstance abuse.
- Mental Health Benefits: Emerging research indicates ibogaine may alleviate symptoms of depression, anxiety, and post-traumatic stress disorder (PTSD), particularly when paired with psychotherapy, offering a holistic approach to recovery.
Despite these benefits, ibogaine is not without risks. Its use is associated with cardiac complications, including QT-interval prolongation, which can lead to arrhythmias or, in rare cases, sudden death. These risks underscore the need for medical supervision during treatment.
Ibogaine Therapy and Psychedelic Treatments in Canada
In Canada, ibogaine occupies a legal gray area. It is not explicitly scheduled under the Controlled Substances Act, but since 2017, Health Canada has listed it on the Prescription Drug List, meaning it can only be accessed with a doctor’s prescription. However, it lacks formal approval as a therapeutic drug, and its use remains rare within conventional medical settings. Despite this, underground and semi-legal clinics have emerged, particularly in British Columbia and Ontario, catering to individuals seeking alternatives to mainstream addiction treatments.
Canadian ibogaine therapy typically involves a single high-dose session (10-20 mg/kg), administered orally as ibogaine hydrochloride under medical supervision. The experience unfolds in two phases:
- Visionary Phase (4-6 hours): Patients enter a waking dream state, often reliving past events or confronting suppressed emotions. This phase is intensely introspective and can be emotionally taxing.
- Introspection Phase (up to 20 hours): A period of reflection follows, during which patients process insights gained during the visionary phase, often reporting a renewed sense of purpose or clarity about their addiction.
Post-treatment, patients are encouraged to engage in psychotherapy or aftercare programs to integrate their experiences and sustain sobriety. Clinics in Canada often combine ibogaine with magnesium infusions to mitigate cardiac risks, a practice informed by recent studies on veterans with traumatic brain injuries.
The opioid crisis, which claimed over 40,000 lives in Canada between 2016 and 2023, has fueled interest in ibogaine therapy. Advocates argue it could complement existing treatments like methadone or buprenorphine, which often fail to address the psychological underpinnings of addiction. Small-scale observational studies, such as those funded by the Multidisciplinary Association for Psychedelic Studies (MAPS), have reported success rates of 30-75% for opioid cessation following ibogaine treatment, far surpassing the 8-35% efficacy of opioid replacement therapies.
Efforts to Legalize Ibogaine in Canada
The push to legalize ibogaine in Canada reflects a broader psychedelic renaissance, with substances like psilocybin and MDMA gaining traction for therapeutic use. Key efforts include:
- Advocacy by Organizations: Groups like MAPS Canada and the Canadian Psychedelic Association are lobbying for ibogaine’s reclassification, citing its potential to address the opioid epidemic. They emphasize the need for regulated clinical trials to establish safety and efficacy.
- Research Initiatives: Canadian universities, such as the University of British Columbia, are exploring ibogaine’s mechanisms, though funding remains limited due to its legal status. In 2024, a pilot study in Vancouver began recruiting participants to assess ibogaine’s effects on opioid dependence, signaling growing academic interest.
- Public Sentiment: Posts on X and media reports, such as a March 2025 CBC feature, highlight increasing public and professional support for ibogaine, with addiction specialists and recovered users touting its benefits. However, skepticism persists due to safety concerns and a lack of large-scale data.
- Policy Proposals: In 2023, British Columbia decriminalized possession of small amounts of illicit drugs, opening the door to alternative treatment discussions. Advocates have proposed ibogaine pilot programs, similar to those attempted in U.S. states like Vermont and Maryland, though no legislation has yet passed.
Health Canada’s cautious stance reflects a balancing act between innovation and risk. Legalization would require rigorous clinical trials, standardized protocols, and safeguards against misuse—steps that could take years to implement.
Sourcing Ibogaine: From Africa to Clinics
Ibogaine is primarily sourced from the root bark of Tabernanthe iboga, a shrub native to Gabon and surrounding regions. Harvesting involves stripping the bark, drying it, and extracting ibogaine through chemical processes, yielding either a crude powder or purified ibogaine hydrochloride. The plant’s slow growth and limited geographic range raise sustainability concerns, as demand for ibogaine therapy grows globally.
In Gabon, iboga is a cultural treasure, but overharvesting has prompted calls for regulation. Some clinics source ibogaine from cultivated plantations in South Africa or Costa Rica, where it is grown under controlled conditions to meet international demand. Synthetic ibogaine, produced in laboratories, is another emerging option, though it remains cost-prohibitive and less common.
Once sourced, ibogaine is processed into capsules or solutions for clinical use. In Canada, underground providers often import it from countries like Mexico or New Zealand, where it is unregulated, navigating a complex web of international trade and customs laws.
Usage and Effects on Addiction Recovery
Ibogaine’s administration is highly controlled due to its potency and risks. Before treatment, patients undergo medical screening, including ECGs to assess cardiac health, and are monitored throughout the session by trained professionals. The process typically occurs in a residential setting, lasting 24-48 hours, followed by rest and integration support.
The effects on addiction recovery are multifaceted:
- Pharmacological Action: Ibogaine interacts with multiple neurotransmitter systems—serotonin, dopamine, and opioid receptors—resetting pathways altered by chronic substance use. Noribogaine, its long-acting metabolite, sustains these effects, reducing relapse risk.
- Psychological Transformation: The visionary experience often reveals the emotional or traumatic roots of addiction, empowering patients to confront and reframe their behaviors. For example, a patient might relive childhood abuse, gaining closure that diminishes the urge to self-medicate.
- Long-Term Outcomes: Observational studies report sustained abstinence in 30-60% of patients one year post-treatment, with higher success rates when paired with aftercare. A 2018 New Zealand study found 75% of participants remained opioid-free after 12 months, though sample sizes were small.
For substance abuse, ibogaine’s ability to break the cycle of compulsive use is its hallmark. Unlike maintenance therapies, it offers a one-time intervention that can reset both body and mind, though its efficacy varies by individual and substance type.
Ibogaine’s Promise and Perils
Ibogaine represents a convergence of ancient wisdom and modern science, offering a radical approach to addiction recovery. Its history as a sacred plant and its emerging role in psychedelic therapy highlight its potential to transform lives, particularly in Canada, where the opioid crisis demands innovative solutions. Efforts to legalize it face hurdles, but growing research and advocacy may pave the way for regulated use.
Sourced from African roots or synthesized labs, ibogaine’s journey to the clinic is fraught with ethical and logistical challenges. Yet, its ability to alleviate withdrawal, curb cravings, and foster profound psychological shifts makes it a compelling candidate for addressing substance abuse. As Canada navigates its legal and medical future, ibogaine stands as both a beacon of hope and a call for cautious, evidence-based exploration.
Always consult an informed healthcare professional or your family doctor when considering any medication or therapy.

For more information or to reach out to us visit our website or email us at drphillocybin@gmail.com
